The diagnosis of melanoma is mainly performed through an excisional biopsy, even if the dermatologist is able to determine the presence of a suspected melanoma through an accurate anamnesis, a clinical inspection and with diagnostic tests.

The medical history is extremely important, the patient can provide us with information on any other cases of melanoma in the family, and also provides us with information on when the suspicious growth appeared and on how it behaved (increase in size in the short term, change of color, shape change). Already a careful inspection by the dermatologist can lead to a diagnosis of melanoma or suspected melanoma, but nowadays the development of dermoscopy or epiluminescence microscopy allows the dermatologist to arrive more and more at a precise and early diagnosis which obviously will then be confirmed by a histological examination associated with the immunohistochemical study of the histological preparation.

Furthermore, the use of computerized systems for archiving dermatoscopic images makes it possible to carefully evaluate the changes in pigmented lesions over time and therefore to arrive at extremely early diagnoses. In the diagnostic field it is extremely important to remember that there are melanomas that are difficult to identify such as amelanotic melanoma which often appears as a non-pigmented nodular lesion, in these cases the dermatoscopic examination almost always allows the identification of morphological alterations suspected of melanoma. Three other methods have been studied for the study of melanoma, but more results still need to be obtained before they can be used in daily clinical practice:
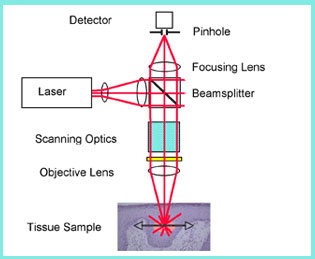
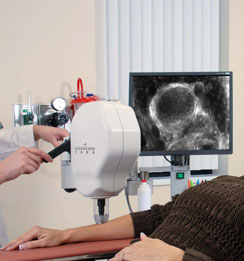
Confocal microscopy: this method uses a low power laser beam to obtain detailed images of suspicious lesions, giving the dermatologist an almost cellular vision of the lesion. It allows, through an infrared light emitted by a low power laser, to highlight the tissues. The reflected laser light comes back as a bright image that contrasts with a dark image that corresponds to the light-absorbing parts. The contrast between bright images (reflected light) and dark images (absorbed light) give an image similar to that of a histological examination. The confocal microscope is able to magnify it more than 700 times, thus showing its cellular structure, without the need to remove it surgically. With the new diagnostic method, diagnostic accuracy reaches 98% and the need to perform biopsies on benign lesions is reduced by 23% and removals in general by 60%. few centers use the tool.

Optical coherence tomography: mainly used in ocular lesions. Reflex transmission imaging: it is an ultrasound examination and is used for the study of lesions of the eye and which has been seen to help in the early detection of melanoma. Bibliography: Casagrande Tavoloni Braga J, Scope A, Klaz I et al. “The significance of reflectance confocal microscopy in the assessment of solitary pink skin lesions.” Journal of the American Academy of Dermatology 2009. Goodson AG, Grossman D. “Strategies for early melanoma detection: Approaches to the patient with nevi.” Journal of the American Academy of Dermatology 2009; 60: 719-35; quizzes 36-8. Segura S, Puig S, Carrera C et al. “Development of a two-step method for the diagnosis of melanoma by reflectance confocal microscopy.” Journal of the American Academy of Dermatology 2009.